Mount Pleasant, S.C. – Sharon Bridges has been depending on Medicaid for her health care needs since 1998. But now, in the middle of a serious medical condition, she has been suddenly cut off from coverage without warning. Sharon is now unsure how she’ll survive as she faces treatment for thyroid cancer.
Cut Off Without Notice
Bridges found out about the cutoff in the most shocking way — during a hospital call meant to approve her surgery.
“They called to approve my surgery for June 10,” Sharon said. “That’s when the hospital told me my Medicaid benefits had ended on May 1.”
This came as a complete surprise to her. She had no idea her Medicaid had been stopped and says she didn’t receive any proper notification.
Life-Saving Medication at Risk
Sharon is being treated for thyroid cancer and already had part of her thyroid removed. She’s currently being monitored for signs of cancer spread and low calcium levels in her body — both of which are serious concerns.
“I take three different calcium supplements every day,” she said. “On Monday, I was supposed to take an injection that I couldn’t get because I don’t have access to the medicine anymore.”
She also has a body scan and ultrasound scheduled for July, which are important for checking her condition. Without these, her health could worsen quickly.
“If I can’t see my doctors and get my levels checked, they’ll drop and eventually I’ll die,” Sharon said emotionally. “My grandbaby was just born, and I should be celebrating that. But instead, I’m scared about staying alive.”
Confusing and Inaccurate Reasons
Bridges said that when she contacted Medicaid, she was given several reasons for the cutoff — all of which she insists are incorrect.
“They told me someone named Martin was added to my household,” she said. “But I’ve never had anyone named Martin living with me.”
She believes this error is what caused the cancellation, but she’s struggling to get the issue resolved.
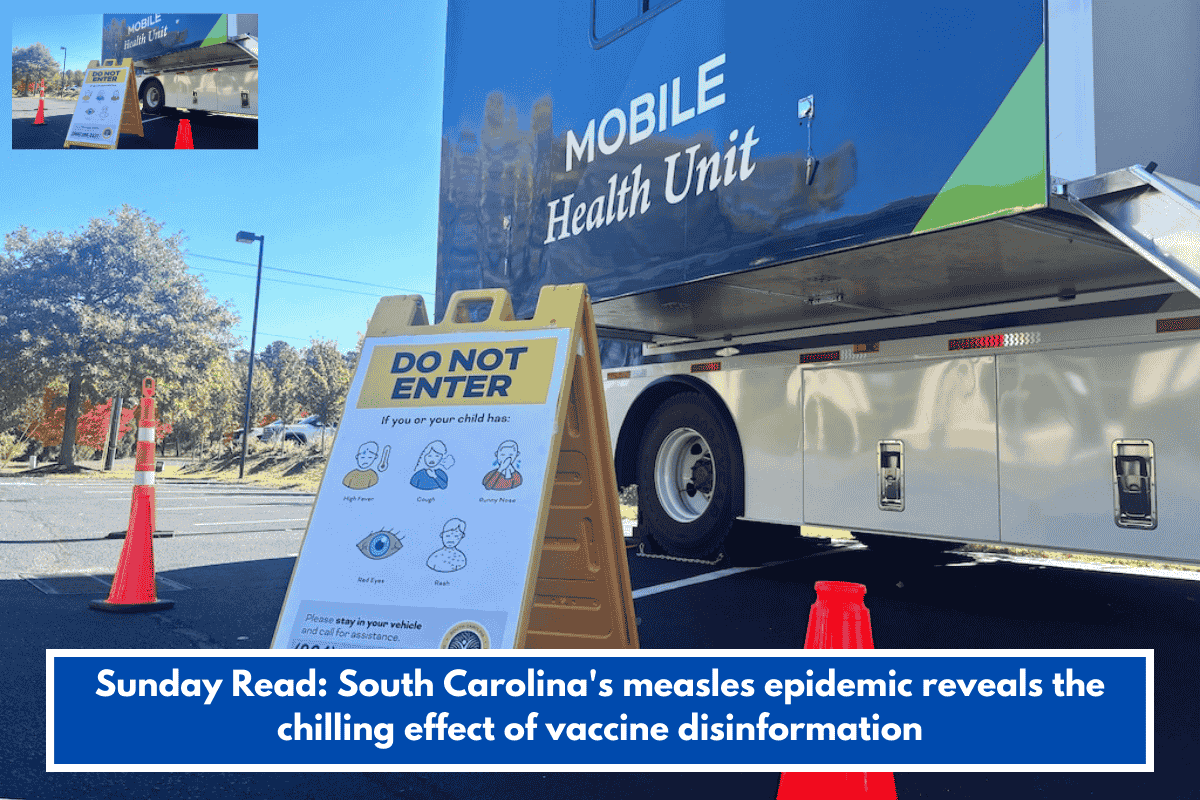
Why This Is Happening to Others Too
According to Shelly All, a Medicaid lawyer, Sharon’s case is not unique. Many people are losing Medicaid coverage after COVID-19 pandemic policy changes, especially now that annual reviews have restarted.
During the pandemic, annual eligibility checks were paused to keep people from losing benefits. But now that those checks are back, people are being dropped — sometimes wrongly.
What You Can Do If Medicaid Cuts You Off
Lawyer Shelly All shared some advice for those in a similar situation:
“First, talk directly to a caseworker at Medicaid and find out the reason for the change in eligibility,” she said.
If that doesn’t help, All suggests contacting legal support services, such as Charleston Legal Aid, or looking for pro bono legal assistance.
“They may be able to help file an appeal or find another solution to keep you covered,” she said.
Sharon Bridges is just one of many facing the real-life consequences of Medicaid errors or misunderstandings. Her story is a powerful reminder of the importance of clear communication and proper reviews when it comes to healthcare.
As people across South Carolina and the country continue to adjust after the COVID-19 changes, it’s important to double-check Medicaid status, follow up with caseworkers, and ask for help early if something doesn’t seem right.
Sharon’s fight is not just against cancer — it’s now a fight for access to the care that could save her life.